How Spiras Health Integrates SDoH into Whole-Person Care
By dr-david-hagaman-chief-medical-officer | August 8, 2023

A small population of the sickest patients drives a sizeable portion of the nation’s healthcare spending. This imbalance is further magnified by the impact of social determinants of health (SDoH) on chronic disease.
SDoH factors make it harder for people with multiple conditions to engage in healthy behaviors, access all resources available to them for their healthcare, and keep their symptoms under control.
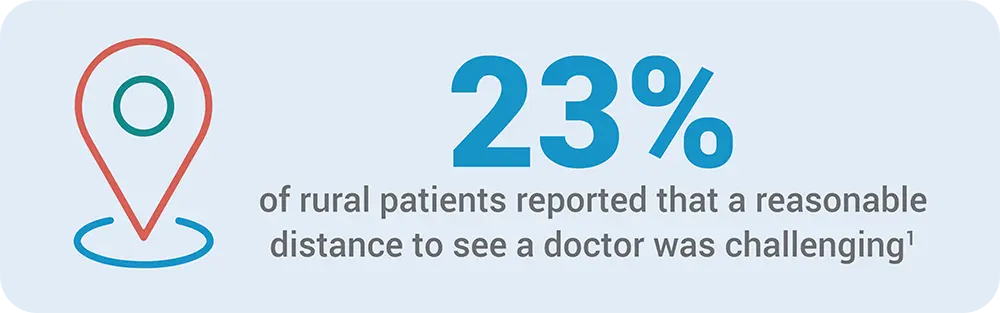
For a patient living with multiple chronic conditions, the simple fact of geography impacts their health. For example, rural patients may be unable to access care simply because of the distance to a medical facility. A 2018 Pew survey found that 23 percent of rural patients reported that a reasonable distance to see a doctor was challenging.1
Other non-medical factors hinder positive health outcomes. If a patient is not taking blood pressure medicine regularly because he can’t afford it, his pressure is not likely to be well-controlled, and his condition is likely to deteriorate.
SDoH has become a hot topic across the healthcare arena and at industry conferences for these reasons. But for me and my team, it is more than a buzzword – managing health-related social needs is a natural part of our care. Since our inception, Spiras Health has delivered whole-person care to our patients’ homes.
In one example, one of our nurses visited a patient in Indiana to discover that her walls and carpet were waterlogged in the aftermath of a spring flood, leaving her living on an enclosed porch. One of our first steps of care was to find her safe housing.
The link in the chain of care
At Spiras Health, we consider ourselves an important link in the chain of care because we treat patients in their homes where social needs are real sources of stress – financial, emotional, behavioral, and environmental – that affect the whole person.
When we come into the home, we notice the empty prescription bottles, what kind of food is in the kitchen, or if the patient wants to be outside of the house away from the spouse to receive a phone call. If the house is 90 degrees inside, we ask if they have trouble paying the power bill. For patient appointments, we check on their transportation and encourage their attendance.
The value of whole-person care in the home
Our mission is to deliver home-based care to patients at risk of an emergency event or hospitalization. Instead of an episodic approach that solely leans on office check-ups and ER visits, Spiras Health uses a longitudinal model to augment PCP and Specialist care. We are positioned to recognize and track changes in condition and keep patients as stable as possible while improving their overall healthcare experience.
Our care team is not a substitute for PCP care but is an extension of care between visits. As the home-based eyes and ears for the health plan and PCP, our nurse practitioners can diagnose, treat, and prescribe medicines, which are particularly helpful for emerging exacerbations. We also consult with the PCP to develop a care plan and ensure that each patient gets the medical attention their conditions require.
Treating the Lived Experience
My conversations with our health plan partners focus on social factors that impact a member’s prognosis and the best way to uncover their social needs. We use a screening tool and workflow adapted from PRAPARE, the national standard, to ensure that our trained observations flow seamlessly into our EMR.
Even with the latest screening tools, we’ve come to an understanding that only a trained nurse can observe and recognize SDoH factors first-hand.
When we sit with a member, we use this time to develop a bond of trust where they can share concerns about financial issues, food insecurity, money for medications, transportation to appointments, health literacy, caretakers, and loneliness and isolation. We also look for environmental risks, including fall risks, HVAC or refrigerator issues, and mold.
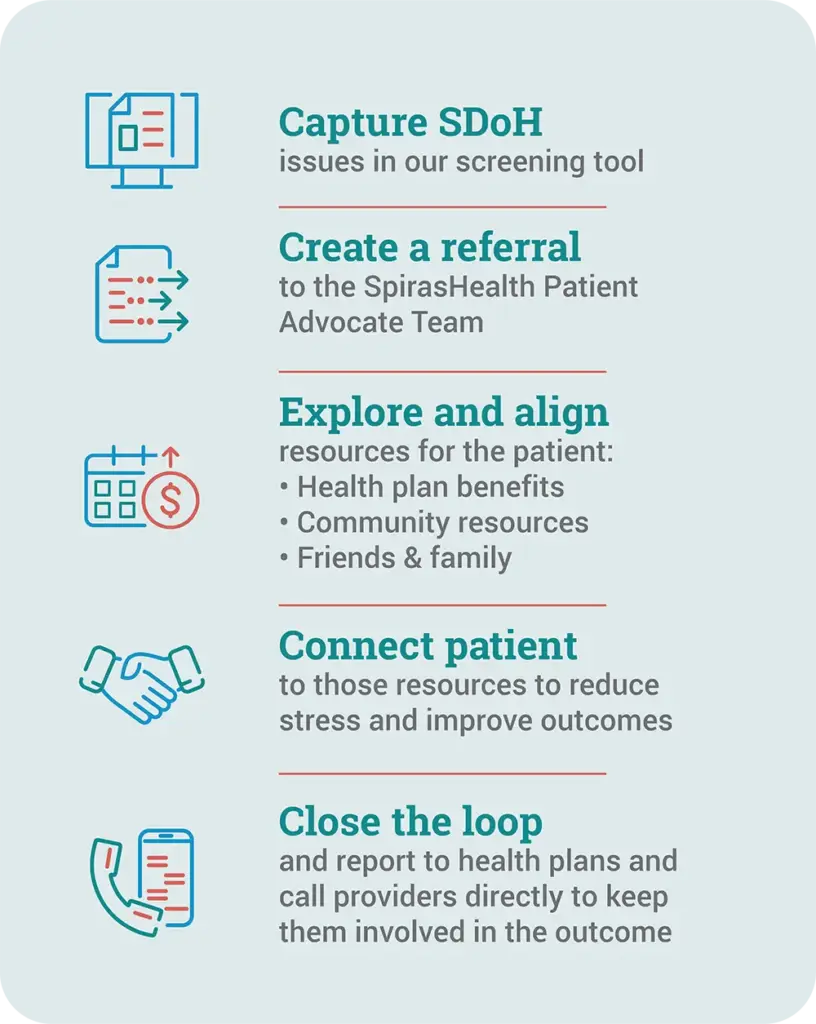
Our model for “closing the loop”
The challenge for health plans and providers is to find partners who can “close the loop” and solve the patient’s social needs, not just identify them.
Home Health Care News recently featured Spiras Health, describing our approach as “a proprietary predictive model, personalized care planning, and attention to social determinants of health (SDoH).” 2 This model is founded on the fact that home-based nurses are positioned to see those needs, know the family, and connect patients to community resources and health plan benefits:
SDoH stories
Recently, one of our nurses, Jessica Knopp, learned that her patient forgets to take medications or, even worse, takes them twice. The patient would pull a pill bottle out of a white bag, take the med, put it back, and lose track. Jessicacame up with a system. She now fills four weekly med planners from the white bag and puts the accessed bottles into an additional red bag. At the end of the month, Jessica refills the planners – from red to white – an example of how an on-site nurse prevented medication problems with a simple solution.
Often, patients have social needs that can be solved using their existing health plan benefits. One of our patients was living on less than $100 monthly for food. Our nurse asked him about his benefits and discovered that he had an expired benefit card — a pre-loaded debit card that can be used to buy healthy food, over-the-counter health products, and even pay utility bills. He was unaware of how to use it, so we contacted the health plan and arranged for a new card to get him started. During a follow-up, the patient was extremely thankful to be able to eat well and not worry about running out of food before the month’s end.
The clinical impact of whole-person care
The industry is beginning to show positive results from SDoH efforts, for example, improving medication adherence or solving for medicine co-pays. These efforts help patients avoid the ER and keep them on track with their conditions. Our trusted clinicians become like clinical family members, dependable resources who help patients understand and progress toward more engagement in their own health care.
At Spiras Health, we help patients make better choices and changes impacting their quality of life. This whole-person approach combines their physical health needs and social concerns through a better understanding of a person’s lived experiences, the people in their life, and what’s meaningful to them. This relatively small portion of the sickest patients deserves our best efforts and rewards those efforts with improvements that make a world of difference to their experience of healthcare and enjoyment of life.
To learn how to offer Spiras Health to your members with complex needs, contact us using the form below
- www.pewsocialtrends.org/2018/05/22/views-of-problems-facing-urban-suburban-and-rural-communities/
- homehealthcarenews.com/2023/07/behind-spiras-healths-strategy-to-uncover-address-care-gaps-in-the-home/

 Prev
Prev