New Options for Managing RSV Risks in Polychronic Populations
By dr-david-hagaman-chief-medical-officer | September 27, 2023
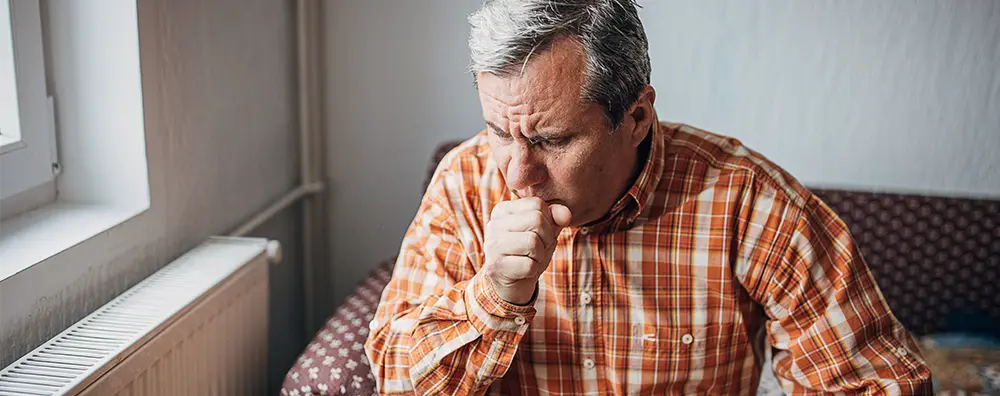
Respiratory syncytial virus (RSV) has attracted attention as one part of the ‘tripledemic’ that populated news headlines last winter, and recently because of new vaccine availability. RSV causes mild cold symptoms in most people but can lead to more severe infections such as bronchitis and pneumonia, causing hospitalization and even death in older people and those with weakened immune systems.
What is RSV?
RSV is a seasonal illness, typically starting in the fall and peaking in the winter. Once a person is infected, the usual treatment is supportive care, such as over-the-counter medications and maintaining hydration. Most people get better in a week or two due to strong immunity from a lifetime of multiple exposures. As people age, however, they lose their ability to ward off infection.
RSV spreads by:
- Inhaling droplets when infected people cough or sneeze. Experts indicate that masks protect you from many common respiratory illnesses, including RSV.
- Touching a surface that has droplets from a cough or a sneeze from an infected person. If you touch that surface, and then touch your nose, mouth, or eyes, you could get infected. You can kill RSV by cleaning your hands with soap and water or with an alcohol-based hand sanitizer.
But when RSV makes its way down into the lungs, causing lower respiratory tract disease (LRTD), it can cause vulnerable people, including those 65 and older, to develop life-threatening complications, such as pneumonia, and make existing conditions, such as asthma, congestive heart failure, and chronic obstructive pulmonary disease (COPD), worse. Each year, this leads to 60,000 to 160,000 RSV hospitalizations in adults 65 and older, and 6,000 to 10,000 deaths (View source data at cdc.gov ).
During the COVID pandemic, when people were being very careful with cleanliness, wearing masks and distancing, there was a decrease in RSV infections. Now that those restrictions have loosened, we are seeing an increase in RSV infections. However, two new RSV vaccines aimed at older people are now available this fall.
What vaccines are available?
In June, the Centers for Disease Control and Prevention (CDC) confirmed the Food and Drug Administration (FDA)’s approval of the two vaccines for older people, specifying that those ages 60 and older may get them based on shared clinical decision-making. This means they may receive a single dose based on discussions with their health care provider about whether RSV vaccination is right for them.
Both vaccines for older adults use traditional platforms — like a flu shot (not to be confused with the mRNA technology introduced by Pfizer-BioNTech and Moderna to prevent COVID-19). The RSV vaccines work by introducing an inactivated RSV protein into the body, where it stimulates the immune system to help the body fight off the RSV virus and prevent severe disease.
Both vaccines performed well in clinical trials, according to data presented to the FDA. Arexvy™, developed by GSK, was the first to receive FDA approval — in early May — based on data from a trial the company conducted in the U.S. and internationally. The ongoing trial is following participants through three RSV seasons. In late June, GSK reported an overall efficacy of 82.6% against LRTD during the first season, 77.3% for mid-season, and 67.2% over two seasons. Against severe disease, efficacy was 94.1% during the first season, 84.6% at mid-season, and 78.8% over two seasons.
The second vaccine, Abrysvo™, developed by Pfizer, showed an efficacy of almost 89% against LRTD involving at least three symptoms in the first year after vaccination, and 78.6% midway through a second season in the data presented to the FDA. LRTD symptoms include new or increased cough, wheezing, sputum (phlegm) production, shortness of breath, and/or tachypnea (abnormally rapid breathing).
What are potential side effects?
The vaccines made by GSK and Pfizer have similar side effects. Most common side effects are mild and go away after a few days. People who had the vaccines reported:
- Pain where they received the shot
- Fatigue (feeling more weak or tired than usual)
- Headache
- Muscle pain
The CDC advisory panel expressed concerns about the clinical trial data, to the point where they changed an initially strong recommendation to get the vaccine, if eligible, to one that states people over 60 ‘may’ get an RSV vaccine based on a shared discussion with their doctors. For some, this may mean a discussion with their pharmacist. (The RSV vaccines will be covered by Medicare Part D and, thus, will be administered in pharmacies in many cases).
One issue was that a few people in the trials developed Guillain-Barré syndrome in the days following the shot. Guillain-Barré is a rare disorder that causes muscle weakness and sometimes paralysis.
In addition, atrial fibrillation (an arrhythmia that can lead to blood clots in the heart) within 30 days of vaccination was reported in 10 participants who received Arexvy and four participants who received a placebo.
Another issue was that most of the participants in the clinical trials were in their 60s, so there was little data on other high-risk groups, such as those over age 80.
Who could benefit from the vaccine?
The benefits of the new vaccines for older adults outweigh the potential harms in cases where RSV could be life-threatening. It is recommended for all eligible older adults, particularly those with underlying health conditions, such as heart or lung disease, or weakened immune systems.
They also suggest that people who are vulnerable or could infect others who are at high risk take additional precautions this fall. Since RSV is spread through contact with contaminated surfaces, that includes washing hands often, keeping hands away from your face, avoiding kissing and other close contact with people who have cold-like symptoms, cleaning frequently touched surfaces, such as doorknobs and mobile devices, and staying home when you are sick.
What is the right timing for the vaccine?
Should you get a COVID booster, flu vaccine, and RSV vaccine all at once, if you are eligible?
Experts are still working to answer that question— and so far, the data is still limited. But the FDA and CDC will continue to monitor the vaccines. According to the New York Times, the CDC is expected to make recommendations on administration of the three vaccines together in the coming weeks.
To learn how to offer Spiras Health to your members with complex needs, contact us using the form below
David Hagaman, MD, is a pulmonologist and Spiras Health’s Chief Medical Officer and Co-Founder. Additionally, he is a member of the faculty at the Vanderbilt University School of Medicine as well as the Medical Director of Outreach at Vanderbilt University Medical Center’s Asthma, Sinus and Allergy Program.

 Prev
Prev